

Belly fat deadlier than obesity, study finds
PEOPLE who weigh a normal amount when they step on the scale may be at higher risk of dying in the medium term if their fat is concentrated in the abdomen, say doctors who want everyone to use a tape measure to measure themselves.
Researchers have long suspected the body mass index or BMI, that tells you how appropriate your weight is to your height is not a good measure of body fatness — particularly fat that accumulates in the belly and within abdominal organs and leads to inflammation, glucose intolerance and other complications that increase the risk of cardiovascular disease and Type 2 diabetes.
The study was published in Monday’s issue of the scientific journal Annals of Internal Medicine.
“There are many different names for it,” said study co-author Thais Coutinho, a cardiologist at the Ottawa Heart Institute. “There’s the apple shape as opposed to the pear shape, there’s a muffin top, there is a beer belly. A spare tire. But basically, it is exactly what it sounds like: if somebody has a disproportionately large abdomen compared to other parts of the body.”
Coutinho and her co-authors from the Mayo Clinic in Rochester, Minnesota, United Sta assessed the five- and 10-year mortality risk in men and women with normal BMIs and central obesity compared with those who are overweight or obese based on BMI. The study included more than 15,000 participants who were followed for an average of 14.3 years as part of the U.S.-based Third National Health and Nutrition Examination Survey, known as NHANES III.
“We found that the group of patients that actually has the highest risk of dying were precisely the patients who had normal BMI, so these are people who are not necessarily heavy for their height, but they were centrally obese,” Coutinho said.
For a man with central obesity and normal BMI, the mortality risk was double that of those who were overweight or obese based on BMI alone. For women with central obesity and normal BMI, the mortality risk was nearly 1.5 times greater than for those with a problematic BMI but without fat concentrated in the middle.
Raj Padwal, a physician at the University of Alberta’s faculty of medicine who studies cardiovascular risks and obesity, said the results show “it’s not just how much fat you have, but it’s where the fat is.”
“The worst fat is in the midsection. It’s in the intra-abdominal cavity, in the organs,” Padwal explained. “Fat infiltrating that area of the body is definitely the worst in terms of future risk of cardiovascular complications and future risk of death.”
That’s because central obesity is linked to fat infiltrating the pancreas and liver, which in turn is linked to risk of Type 2 diabetes, fatty liver and eventually end-stage liver failure, he said.
Padwal said BMI has served its use and should no longer be used clinically. “Preferentially, I would say waist-hip ratio or waist circumference should be measured and BMI should be discarded.”
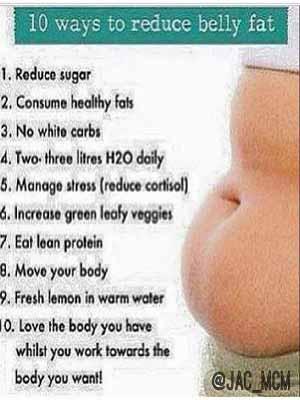
The study’s authors said their findings suggest those with normal weight, but central obesity could be an important population to target for prevention and lifestyle changes.
While long-term weight loss is notoriously difficult, Coutinho said healthy lifestyle changes bring positive changes in the body regardless of fat loss, such as lower blood pressure.
To calculate your waist-to-hip ratio, measure your waist at its narrowest, and then divide that by the measure of your hips at their widest.
If the result is greater than .85 in women or greater than .90 in men, then lifestyle and exercise changes are recommended to improve health in the long run.
“It’s very simple. It’s just a tape measure,” she said. “Everybody can do and it can help us identify people at highest and lowest risk.”
There is also equipment to give a more sophisticated measure of fat directly, but doctors face a trade-off between what’s pragmatic and what’s the best measurement, Padwal said.
Meanwhile, patients with type 2 diabetes and high blood pressure have a significantly increased risk of heart attacks and strokes. As such, research into methods that minimize these risks is vital.
Individuals with a systolic blood pressure of 140 or more are considered to have high blood pressure.
In 2010, hospitalization rates for stroke were 1.5 times higher among adults with diabetes aged 20 years or older, compared with the general population. Research into effective methods of controlling blood pressure is increasingly valuable as the obesity trend continues.
These new findings were presented at the American Heart Association’s Scientific Sessions 2015. The team of investigators, from Melbourne, Australia, found that just a few minutes of light movement every 30 minutes could lower blood pressure.
Source: TheGuardian
Share this post
Naijanetwork Forum Statistics
Threads: 14843,
Posts: 17902,
Members: 6711


